Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding the correct leads ecg placement is crucial for accurate cardiac diagnostics. A small error can lead to misdiagnosis, delayed treatment, or unnecessary tests. Let’s dive into the essentials every healthcare provider and student must know.
What Is Leads ECG Placement and Why It Matters

Electrocardiogram (ECG) testing is one of the most widely used diagnostic tools in cardiology. At the heart of this test lies the precise positioning of electrodes on the patient’s body—commonly referred to as leads ecg placement. Proper placement ensures that the electrical activity of the heart is recorded accurately across multiple leads, providing clinicians with vital data about rhythm, conduction, ischemia, and structural abnormalities.
Incorrect leads ecg placement can distort waveforms, mimic pathology, or mask real conditions. For example, misplaced precordial leads can create false impressions of myocardial infarction or ventricular hypertrophy. According to the American Heart Association (AHA), up to 40% of routine ECGs contain lead placement errors, significantly affecting diagnostic reliability (Circulation, AHA).
Anatomy Behind ECG Leads
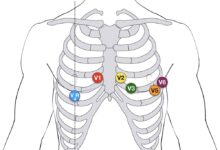
The standard 12-lead ECG uses 10 electrodes placed at specific anatomical landmarks to generate 12 different electrical views of the heart. These include six limb leads (I, II, III, aVR, aVL, aVF) and six precordial (chest) leads (V1–V6). Each lead observes the heart from a unique angle, capturing depolarization and repolarization sequences.
The limb leads are derived from electrodes on the arms and legs, while the precordial leads are positioned across the chest wall in precise intercostal spaces. The spatial orientation of these leads allows for a three-dimensional assessment of cardiac electrical activity.
- Limb leads assess the frontal plane of the heart.
- Precordial leads evaluate the horizontal (transverse) plane.
- Each precordial electrode corresponds to a specific region of the myocardium.
“Accurate lead placement is not just technique—it’s diagnostic integrity.” – Journal of Electrocardiology
Standardization: The AHA and ESC Guidelines
The American Heart Association (AHA), European Society of Cardiology (ESC), and other international bodies have established standardized protocols for leads ecg placement. These guidelines aim to ensure consistency across clinical settings and reduce variability between recordings.
Key recommendations include using anatomical landmarks such as the sternal angle (Angle of Louis), midclavicular line, and intercostal spaces to guide electrode positioning. For instance, V1 is placed in the fourth intercostal space at the right sternal border, while V4 is located in the fifth intercostal space along the midclavicular line.
Despite these clear standards, studies show poor adherence in real-world practice. A 2020 audit in UK hospitals found that only 58% of ECGs followed correct V-lead placement protocols (European Heart Journal).
Step-by-Step Guide to Correct Leads ECG Placement
Performing a technically sound ECG begins with meticulous attention to detail. Below is a comprehensive, step-by-step approach to ensure accurate leads ecg placement every time.
Limb Lead Placement: Arms and Legs
The four limb electrodes form the basis of the six limb leads. While they are often placed on the wrists and ankles, the AHA recommends placement on the upper arms and thighs to minimize motion artifact and improve signal stability.
Here’s how to position them correctly:
- Right Arm (RA): On the inner aspect of the right upper arm, near the deltoid insertion.
- Left Arm (LA): Corresponding location on the left upper arm.
- Right Leg (RL): On the right lower abdomen or upper thigh—this serves as the electrical ground.
- Left Leg (LL): On the left lower abdomen or upper thigh.
It’s important to note that while distal placements (wrists/ankles) are acceptable, proximal placements reduce baseline wander and interference, especially in ambulatory patients.
“Proximal limb electrode placement improves ECG signal quality and reduces noise.” – AHA Scientific Statement
Precordial (Chest) Lead Placement Sequence
The chest leads (V1–V6) provide critical information about the anterior, lateral, and septal walls of the heart. Their placement must follow a strict anatomical sequence to avoid misinterpretation.
Follow these steps:
- Locate the Angle of Louis (sternal angle) at the second costal cartilage.
- Slide fingers down to the fourth intercostal space at the right sternal border—place V1 here.
- Place V2 at the fourth intercostal space at the left sternal border.
- Place V4 in the fifth intercostal space at the midclavicular line.
- Place V3 midway between V2 and V4.
- Place V5 in the fifth intercostal space at the anterior axillary line.
- Place V6 in the fifth intercostal space at the midaxillary line.
For women with large breasts, it’s recommended to lift the breast tissue to place V3–V6 on the chest wall, not on the breast itself, to prevent signal attenuation.
Using a consistent method like the “V1-V2-V4-V3-V5-V6” sequence helps prevent confusion and ensures accuracy.
Special Considerations for Pediatric and Obese Patients
While standard landmarks apply to most adults, special populations require adjustments in leads ecg placement.
In pediatric patients, the heart is more horizontally oriented and occupies a larger relative space in the thorax. Electrodes should still follow anatomical rules, but technicians must be cautious not to stretch leads excessively. Precordial leads may appear more lateral due to the child’s chest configuration.
For obese patients or those with large breasts, locating intercostal spaces can be challenging. Palpation is key. Use firm pressure to feel rib margins and count spaces carefully. In cases where standard placement is impractical, alternative sites may be used, but this should be documented.
Some institutions use ECG electrode placement guides or templates to assist in difficult cases. These tools can improve consistency, especially among less experienced staff.
Common Errors in Leads ECG Placement and Their Impact
Even minor deviations in leads ecg placement can significantly alter ECG interpretation. Below are the most frequent mistakes and their clinical consequences.
Misplaced Precordial Leads: The Silent Diagnostic Trap
One of the most common errors is incorrect placement of precordial leads, particularly V1 and V2. Placing them one intercostal space too high or too low can mimic or obscure signs of myocardial infarction.
For example:
- Placing V1 and V2 too high may simulate right ventricular hypertrophy or atrial enlargement.
- Placing V4–V6 too high can mimic anterior ST-elevation myocardial infarction (STEMI).
- Laterally displaced V6 may resemble left ventricular hypertrophy.
A study published in Annals of Noninvasive Electrocardiology showed that a 1-inch vertical displacement of V1–V2 altered P-wave amplitude in lead II by up to 30%, potentially leading to misdiagnosis of atrial abnormality.
“A misplaced precordial lead can be as dangerous as a missed diagnosis.” – Annals of Noninvasive Electrocardiology
Reversed Limb Electrodes: A Frequent Yet Avoidable Error
Limb lead reversals, especially right and left arm (RA/LA) reversal, are surprisingly common. This error in leads ecg placement inverts lead I and aVR while altering the appearance of other limb leads.
Classic signs of RA/LA reversal include:
- Inverted P waves, QRS complexes, and T waves in lead I.
- Positive P wave in aVR.
- Lead II and III appear swapped.
This can be mistaken for dextrocardia, but a quick check of lead aVR (which should normally be predominantly negative) can help differentiate. If aVR shows a positive P wave, limb lead reversal is likely.
Other reversals, such as left arm/left leg (LA/LL), can mimic inferior wall myocardial infarction by creating Q waves in leads II, III, and aVF.
Failure to Prepare the Skin Properly
Even with perfect anatomical placement, poor skin preparation can ruin ECG quality. Oils, sweat, hair, and dead skin cells increase electrical impedance, leading to noisy tracings, baseline wander, or missing signals.
Best practices include:
- Wiping the skin with alcohol wipes to remove oils.
- Shaving excessive hair if necessary.
- Gently abrading the skin with gauze to reduce resistance.
- Allowing the skin to dry before applying electrodes.
Failure to do so can result in non-diagnostic ECGs, requiring repeat testing and delaying care.
How Incorrect Leads ECG Placement Mimics Heart Conditions
One of the most dangerous aspects of improper leads ecg placement is its ability to simulate serious cardiac pathologies. Clinicians may initiate unnecessary interventions based on artifact rather than true disease.
Mimicking Myocardial Infarction
Anterior ST-segment elevation is a hallmark of acute anterior MI. However, if V3 is placed too high or too far to the right, it can record signals from the right ventricle, creating false ST elevation.
Similarly, lateral lead misplacement (V5–V6 too superior) can mimic high lateral MI. In one documented case, a patient was nearly taken to the cath lab for suspected STEMI, but the ECG normalized after correcting V4 placement.
Always correlate ECG findings with symptoms, cardiac enzymes, and prior tracings. If the clinical picture doesn’t match the ECG, suspect technical error.
Simulating Ventricular Hypertrophy
Left ventricular hypertrophy (LVH) is diagnosed using voltage criteria in leads like V5, V6, I, and aVL. If chest leads are placed too low, QRS amplitude increases, potentially meeting LVH criteria falsely.
Conversely, placing V1 too low can exaggerate R-wave progression, mimicking posterior MI or right bundle branch block.
A 2018 study in Journal of Electrocardiology found that 22% of false LVH diagnoses were due to lead misplacement.
Creating Arrhythmia-Like Patterns
Lead reversals can generate bizarre axis deviations or abnormal P-wave morphology. For instance, RA/RL reversal may cause extreme axis deviation, resembling ventricular tachycardia.
Additionally, poor contact or floating electrodes can produce intermittent signal loss, creating the illusion of dropped beats or asystole.
“Before diagnosing a rare arrhythmia, rule out lead misplacement.” – Clinical Electrocardiography Textbook
Best Practices for Ensuring Accurate Leads ECG Placement
Accuracy in leads ecg placement is not just about following steps—it’s about cultivating a culture of precision and accountability in clinical practice.
Use Anatomical Landmarks Consistently
The Angle of Louis is the cornerstone of chest lead placement. From this point, you can reliably locate the second rib and count down to the fourth intercostal space for V1 and V2.
Other key landmarks:
- Midclavicular line: Draw an imaginary line from the midpoint of the clavicle downward.
- Anterior axillary line: Follow the anterior axillary fold vertically.
- Midaxillary line: Midpoint between anterior and posterior axillary lines.
Palpate, don’t guess. In obese or edematous patients, take extra time to identify structures by touch.
Train and Re-Train Healthcare Staff
Many ECG errors stem from inadequate training. New nurses, EMTs, and medical assistants often learn placement through observation, not standardized instruction.
Institutions should implement:
- Regular ECG competency assessments.
- Hands-on workshops with mannequins.
- Visual aids posted in ECG rooms.
- Peer review of ECGs for quality control.
A study in Nursing Standard showed that structured training reduced lead placement errors by 67% over six months.
Leverage Technology and Tools
Modern solutions can support accuracy in leads ecg placement:
- ECG electrode templates: Clear plastic guides that overlay the chest to mark correct positions.
- Digital ECG machines with lead monitoring: Real-time feedback on electrode contact quality.
- Mobile apps: Augmented reality tools that guide placement via smartphone camera.
While technology aids, it doesn’t replace clinical judgment. Always verify placement manually.
Special Scenarios: Modified Leads ECG Placement
Not all patients fit the standard model. Certain clinical situations require modifications to conventional leads ecg placement without sacrificing diagnostic value.
Right-Sided ECG for Suspected Right Ventricular MI
In patients with inferior STEMI, right ventricular involvement is a critical consideration. A right-sided ECG involves moving V4R to the fifth intercostal space at the right midclavicular line.
Additional right-sided leads (V1R–V6R) may be used, mirroring the left chest layout. ST elevation in V4R is a strong predictor of right ventricular infarction.
This modified leads ecg placement is essential in acute settings but often overlooked.
Precordial Lead Alternatives in Trauma or Burns
Patients with chest trauma, burns, or surgical dressings may not allow standard electrode placement. In such cases, alternative sites can be used:
- V1–V2: Placed posteriorly at the same level (posterior leads).
- V3–V6: Shifted slightly laterally or to the back, with clear documentation.
While not ideal, these adaptations preserve diagnostic capability when standard placement is impossible.
ECG in Dextrocardia and Situs Inversus
In patients with dextrocardia, the heart is mirrored. Standard leads ecg placement will produce nonsensical results. Instead, a right-sided ECG with mirrored lead placement is required.
For example:
- Place V1–V6 on the right side of the chest in mirror-image positions.
- Reverse limb leads if necessary.
Always confirm dextrocardia with imaging before altering lead placement.
Future of Leads ECG Placement: Innovations and Trends
As technology evolves, so does the methodology behind leads ecg placement. Emerging innovations aim to reduce human error and improve accessibility.
Wearable ECG Devices and AI Integration
Devices like the Apple Watch, AliveCor KardiaMobile, and wearable patches offer single-lead or multi-lead ECGs with minimal setup. While convenient, they often lack the 12-lead comprehensiveness and standardized placement.
However, AI algorithms are being developed to detect lead misplacement automatically. Some systems analyze signal morphology and compare it to expected patterns, flagging potential errors.
For example, GE Healthcare’s Marquette 12SL algorithm includes checks for limb lead reversals and can alert technicians before printing.
Augmented Reality (AR) for Training and Placement
AR headsets and smartphone apps are being tested to overlay correct lead positions onto a patient’s body in real time. These tools use facial recognition and anatomical mapping to guide placement.
Early trials show a 40% reduction in placement errors among novice users.
While not yet mainstream, AR could revolutionize how ECGs are taught and performed, especially in remote or resource-limited settings.
Standardization Through Global Protocols
Despite existing guidelines, global inconsistency persists. Efforts are underway to create unified, digitally accessible protocols with video demonstrations and certification modules.
Organizations like the International Society for Computerized Electrocardiology are pushing for mandatory ECG competency certification for all practitioners involved in ECG acquisition.
Such initiatives could dramatically reduce errors and improve patient outcomes worldwide.
Why is correct leads ecg placement so important?
Correct leads ecg placement ensures accurate recording of the heart’s electrical activity. Errors can lead to misdiagnosis, such as false myocardial infarction or arrhythmia, resulting in inappropriate treatment or delayed care.
What happens if ECG leads are reversed?
Limb lead reversals, especially right and left arm, can invert waveforms in lead I and mimic dextrocardia or inferior MI. These artifacts can lead to serious diagnostic errors if not recognized.
How can I verify correct precordial lead placement?
Use anatomical landmarks: V1 at the 4th intercostal space right sternal border, V2 at the left, V4 at the 5th intercostal space midclavicular line. Place V3 between V2 and V4, V5 and V6 horizontally aligned with V4.
Can ECG lead placement differ in women?
Yes. In women with large breasts, V3–V6 should be placed on the chest wall beneath the breast, not on the breast tissue, to ensure proper signal conduction and avoid distortion.
Are there tools to help with leads ecg placement?
Yes. ECG electrode templates, digital machines with contact monitoring, and AR-based apps can assist in accurate placement. Training and adherence to AHA/ESC guidelines remain essential.
Accurate leads ecg placement is a cornerstone of reliable cardiac diagnosis. From understanding anatomical landmarks to avoiding common pitfalls like limb reversals and poor skin prep, every step matters. As technology advances, tools like AI and AR offer promise for reducing human error. However, the foundation remains proper training, strict adherence to guidelines, and a commitment to precision. Whether you’re a seasoned clinician or a new student, mastering leads ecg placement is not optional—it’s essential for patient safety and diagnostic excellence.
Further Reading: